About IC/BPS
 Patients with interstitial cystitis experience "an unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder" that lasts longer than six weeks in the absence of infection or other identifiable causes. The symptoms can vary greatly between individuals and even for the same person throughout the month, including urinary frequency, urgency, nocturia, pressure and/or pelvic pain. People with severe cases of IC/BPS may urinate as many as 60 times a day.
Patients with interstitial cystitis experience "an unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder" that lasts longer than six weeks in the absence of infection or other identifiable causes. The symptoms can vary greatly between individuals and even for the same person throughout the month, including urinary frequency, urgency, nocturia, pressure and/or pelvic pain. People with severe cases of IC/BPS may urinate as many as 60 times a day.
Physicians may refer to IC with a variety of names, including: bladder pain syndrome (Europe), hypersensitive bladder syndrome (Japan), urologic chronic pelvic pain syndrome (research studies) or chronic pelvic pain syndrome (CPPS). In the United States, it is commonly referred to as IC/BPS.
Pain levels can range from mild tenderness to intense, agonizing pain. Pain typically worsens as the bladder fills with urine and is then relieved after urination. Pain may also radiate to the lower back, upper legs, vulva and penis. Women's symptoms may fluctuate with their menstrual cycle, often flaring during ovulation and/or just before their periods. Men and women may experience discomfort during or after sexual relations.
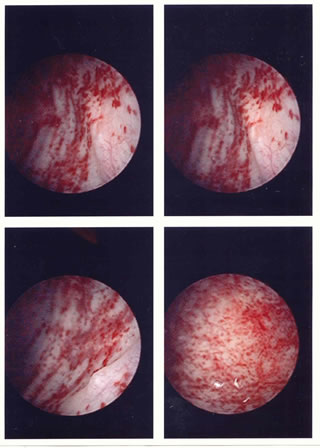
When an IC bladder is closely examined during a hydrodistention with cystoscopy, physicians often find small, bleeding wounds, also known as petechial hemorrhages or glomerulations. About five to ten percent of patients may have larger, more painful wounds known as Hunner's Ulcers. Some patients with mild IC may have bladders that appear normal during a cystoscopy.
In 2009, the RAND Interstitial Cystitis Epidemiology (RICE) study provided astonishing new data on the prevalence of IC in the USA. This National Institutes of Health funded study estimated that 3.4 to 7.8 million women in the USA have symptoms of interstitial cystitis, much higher than was previously thought. Approximately 1 to 4 million men appear to have IC though the true rate has yet to be determined because men are often diagnosed chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) instead. IC can occur in children, teens, young adults and the elderly.
New American Guidelines Released
New American guidelines on interstitial cystitis were released by the American Urology Association earlier this year. The Americans will be using the name Interstitial Cystitis / Bladder Pain Syndrome (IC/BPS) to describe the disorder. The formal definition will be "an unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than 6 weeks duration, in the absence of infection or other identifiable causes."
The committee suggested a five point treatment protocol. Patients should INITIALLY receive good educational materials and outreach, including the introduction of the IC diet principles and general stress and relaxation strategies as needed. After this, a new five step protocol for treatment was suggested:
- First Line Treatments include the use of oral medications including amitryptiline, cimetidine, hydroxzyine and pentosan polysulfate and/or intravesical Instillations including dmso, heparin and lidocaine.
- Second Line Treatments are to be used if no acceptable relief occurs with first line options or if the symptoms suggest a need for a more invasive approach. These include a cystoscopy under anesthesia with a short duration, low pressure hydrodistention and, if present, the treatment of Hunner's Ulcers with fulguration, laser therapy or triamcinolone injection.
- Third Line Treatment include oral cyclosporine and/or the implantation of a neurostimulation device.
- Fourth Line Treatment is the use of Intradetrusor Botox A.
- Fifth Line Treatments are the rarely used surgical methods.
Therapies to avoid included long term antibiotics, intravesical BCG, intravesical RTX, high pressure long duration hydrodistentions and long term oral steroid use. Kegel exercises were also discouraged given the presence of pelvic floor dysfunction in IC.
Read more about the AUA Guidelines here!
Learn more at: http://www.ic-network.com